CMS issues mandatory “TEAM model” for acute care hospitals to improve episode-based alternative payments and promote accountable care relationships | Epstein Becker & Green
(Co-author: Sara Devaraj – Summer Associate)
On August 1, 2024, the Centers for Medicare & Medicaid Services (CMS) published a final rule updating the Medicare Inpatient Prospective Payment System (IPPS) for acute care hospitals and the Medicare Prospective Payment System for long-term care hospitals for fiscal year 2025 (the “Final Rule”).
The final rule includes a new value-based alternative payment model (APM) called the Transforming Episode Accountability Model (“TEAM” or the “TEAM Model”). CMS is expected to issue an official version of the final rule in Federal Register on August 28, 2024.
The TEAM model builds on the CMS Innovation Center’s existing APMs (see Table 1) and advances CMS policy goals by advancing the Innovation Center’s 2021 Strategy Update and 2022 Comprehensive Specialty Care Strategy, which include improving (i) Medicare and Medicaid beneficiaries’ experiences with inpatient and outpatient care and (ii) integrating an accountable care relationship by 2030.
Episode-based payments for acute hospitals
From January 1, 2026, to December 31, 2030, the TEAM Model will test a five-year, mandatory, episode-based APM for acute care hospitals paid under the IPPS. CMS intends to use the TEAM Model to improve beneficiary care through financial accountability for several episode categories, including spinal fusion and major colorectal surgery (see below for the full list of surgeries).
Episode categories for the TEAM model were selected based on feedback from CMS’ 2023 Request for Information (RFI) and are based on their clinical similarity, sufficient volume, and demonstrated success in reducing episode payments to achieve net Medicare savings. As with other episode-based APMs, such as the Bundled Payments for Care Improvement Advanced (BPCI Advanced) model and the Comprehensive Care for Joint Replacement (CJR) model, CMS hopes to be successful in reducing episode payments and achieving net Medicare savings. However, by comparison, TEAM episodes will be strictly surgical-based. TEAM participants will focus on promoting better post-surgical care coordination by connecting patients with primary care physicians and supporting transitions between physicians so that patients recover successfully, avoid hospital readmissions and emergency department visits, and achieve positive long-term health outcomes.
In the TEAM model, an “episode” begins with either an inpatient hospital stay or an outpatient hospital procedure in one of the episode categories listed above. Hospitals participating in the TEAM model must monitor patient care from hospital admission or outpatient procedure through 30 days after the patient is discharged. CMS hopes to test financial accountability for the specified episode categories to reduce Medicare fees for services and maintain quality of care, with the possibility of adding additional episode categories to the model through future notice and comment.
The TEAM model allows for provider and individual integration across most CMS models, which include other advanced primary care models and existing Accountable Care Organizations (ACOs) initiatives (e.g., the Medicare Shared Savings Program and the ACO Realizing Equity, Access, and Community Health (REACH) Model). This would allow an individual assigned to an existing ACO to also be assigned to a TEAM episode if they receive one of the designated surgeries at a participating hospital. CMS believes that “dual assignment” would allow ACO and TEAM participants to collaborate on shared patients and ensure a smooth transition of care between Accountable Care participants.
Participants and geographical area
The TEAM Model will be implemented in 188 geographic areas through the random selection of Core-Based Statistical Areas (CBSAs) delineated by the Office of Management and Budget (OMB) throughout the United States, including CBSAs that have had little previous experience with similar payment models. OMB will also consider areas where safety-net hospitals are located. Acute care hospitals in the selected CBSAs will be required to participate in the model, with limited exceptions. In addition, CMS will allow hospitals participating through the end of BPCI Advanced and CJR to voluntarily participate in the TEAM Model.
Follow the glide path
The TEAM model includes three participation options. Track 1 is a “glide path” that allows participants to transition to full financial risk over time (see Figure A). For participants who need time to prepare for two-sided risk, Track 1 has no downside risk and lower reward levels for the first year of performance (PY) or up to three years for safety-net hospitals. Track 2 will be available in years 2 through 5 for certain hospitals (e.g., rural hospitals, safety-net hospitals, etc.) and will allow for increasing financial risk (two-sided) with quality adjustments to compensation amounts over time. Finally, Track 3 has two-sided financial risk in the form of compensation payments or repayment amounts for years 1 through 5.
By participating in any of these three tracks, TEAM also offers two APM options: (1) an Advanced APM (AAPM) option for TEAM individuals who can demonstrate that they meet the Certified Electronic Health Record Technology (CEHRT) criteria for designation as a Qualifying APM Participant (QP) under the Medicare Quality Payment Program, and (2) a non-AAPM option for TEAM individuals who do not meet the CEHRT criteria. CMS expects TEAM individuals in Tracks 2 and 3 who participate in the AAPM option to qualify as a QP under the Medicare Quality Payment Program.
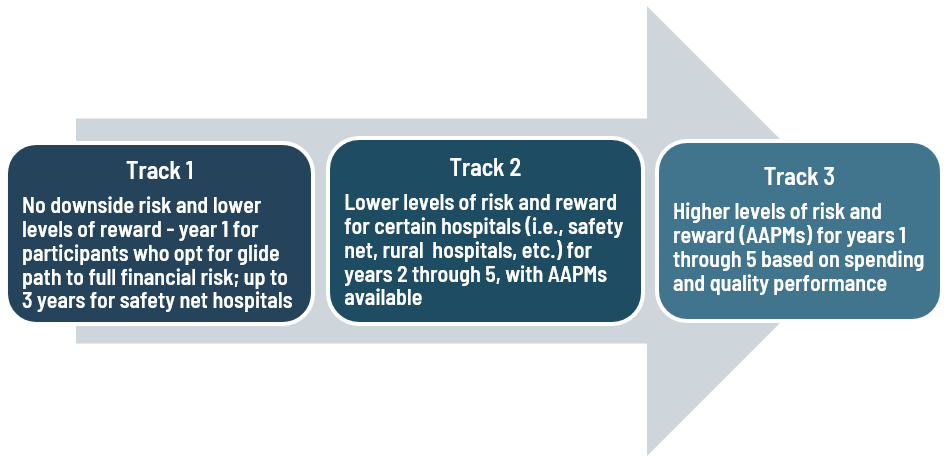
FIGURE A: TEAM Glide Path
Heide Equity
The TEAM model complements CMS’s broader goal of advancing the agency’s health equity strategy by providing flexibility to participating hospitals serving larger numbers of underserved populations by reducing their financial burden associated with participating in the value-based model. The model also calculates a social risk adjustment to ensure that target prices reflect the additional financial investment required to serve underserved beneficiaries. The TEAM model allows hospitals to voluntarily submit health equity plans, report sociodemographic data, and screen beneficiaries for health-related social needs to improve the quality of care.
Decarbonisation and Resilience Initiative
The TEAM model includes a new component called the Decarbonization and Resilience Initiative, which is designed to help hospitals address the impacts of climate change on patient health and health systems and understand how hospital carbon emissions can affect health outcomes, health care costs, and quality of care. This initiative, unique to the TEAM model, marks the first time CMS has included a climate change component in an Innovation Center advanced payment model.
The Decarbonization and Resilience Initiative consists of two parts: (i) technical assistance for all interested TEAM participants and (ii) a voluntary reporting opportunity to collect data on Scope 1 and 2 emissions, which include direct emissions from owned or controlled sources and indirect emissions from purchased energy generation. This initiative provides CMS with the opportunity to gain insight into key decarbonization strategies and improve health system resilience. Ultimately, the goal of the initiative is to generate savings for health systems and the Medicare program. During the comment period, interested stakeholders commenting on the TEAM model most frequently focused on this component and expressed support for the Decarbonization and Resilience Initiative.
Considerations for the future
The TEAM model will have broad implications for various healthcare stakeholders. Hospitals will feel the most immediate impact. By requiring hospitals to participate in the TEAM model, they assume financial responsibility for “episodes” and may need to support change management for physicians and make operational adjustments as a result. This may include working with data analytics and care coordination teams to ensure patients receive high-quality, effective care. Physicians and other healthcare providers may need to increase collaboration with members of the patient’s medical team and change the way care is delivered to ensure their care meets the model’s quality measures.
Please note that stakeholders should review the payment provisions of the final rule themselves, as they contain many other subtle changes to alternative payment systems and other additions.
TABLE 1: Comparison of the CJR and BPCI models with the TEAM model
(View source.)

