MS pharmacists and PBMs disagree over high prescription and business costs
House Committee is unsure what recommendations to make to lawmakers after second meeting on Pharmacy Benefit Managers
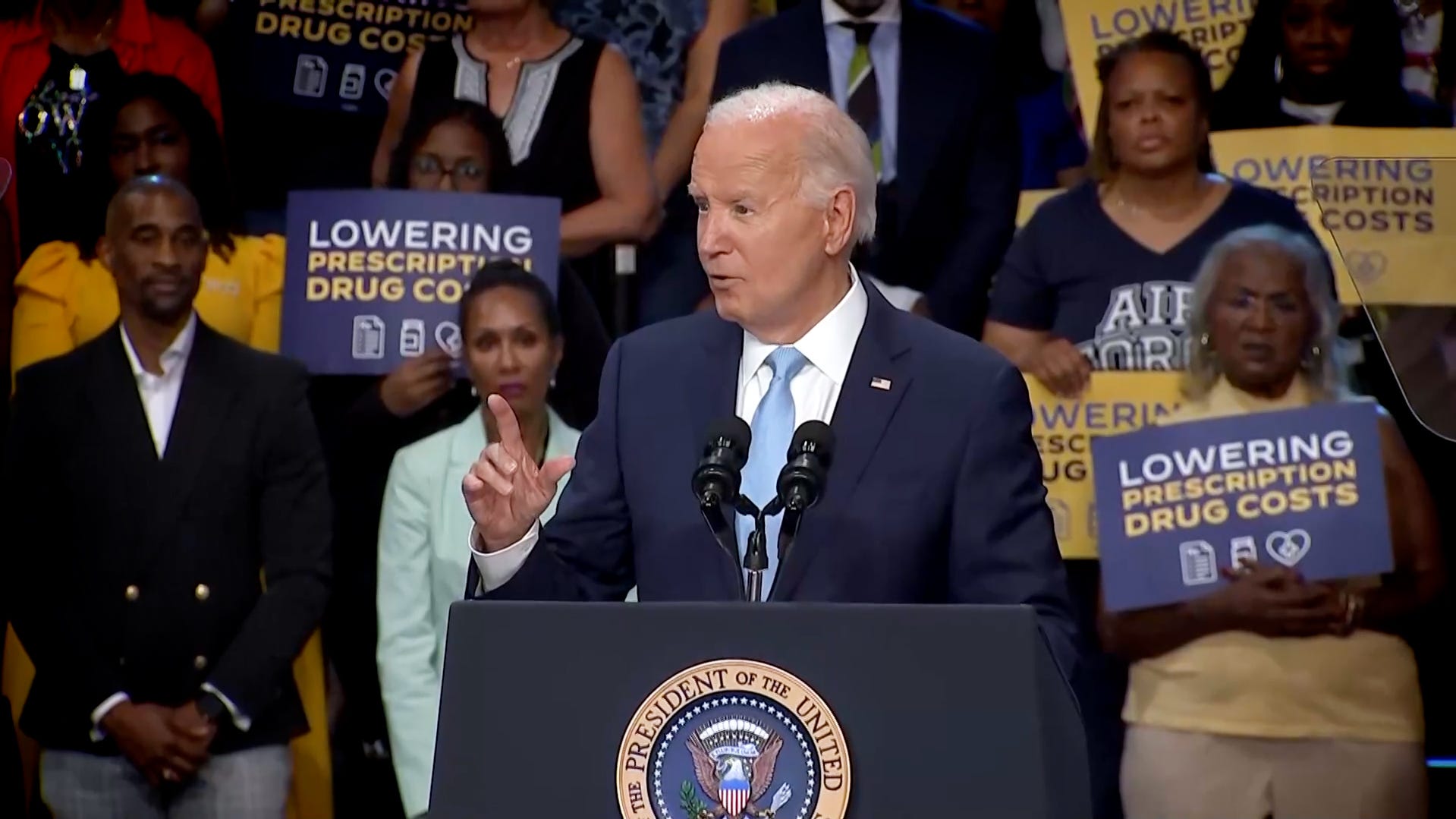
Biden: Medicare has negotiated discounts on 10 prescription drugs
President Joe Biden announced that Medicare had negotiated rebates for ten drugs prescribed to treat blood clots, cancer, heart disease and diabetes.
An attempt by state lawmakers to hear explanations about the rising cost of prescription drugs for patients and pharmacies devolved into a heated exchange on Wednesday between pharmacists, lawmakers and the middlemen who set the purchase and sale prices of the drugs sold to patients.
The problem? If nothing is done, patients could end up paying for increasingly expensive drugs or making longer trips to pharmacies in their care network. The current situation could also leave Mississippi without stronger legal protections, lawmakers and state officials said during a meeting of the House Prescription Drug Policy Taskforce Committee.
“Many people don’t have enough money for gas to drive 25 miles to get their medication,” said committee chairwoman Beth Waldo, R-Pontotoc. “Often it’s a matter of life or death. You need medication.”
Pharmacists believe the core of the problem is the lack of transparency between the prices and contractual terms that these intermediaries negotiate with employers and drug manufacturers and the prices and contractual terms that they negotiate with pharmacies.
These intermediaries are Pharmacy Benefit Managers, whose representatives during the meeting rejected allegations that they were unfair to independent pharmacies, inflated drug prices, favored their own pharmacies and did not negotiate with local pharmacies on drug procurement and pricing terms.
They have left the problems to the Pharmacy Services Administrative Organizations, which represent pharmacies in negotiations with Pharmacy Benefit Managers, drug manufacturers who set the initial price of a drug before it goes on the market, and employers who pay Pharmacy Benefit Managers to negotiate specific prices with pharmacies.
“It’s not in our interest to put these people out of business,” said Tony Grillo, vice president of financial analysis at ExpressScripts, one of the largest pharmacy benefit managers in the country. “This is a critical relationship. The unfortunate part of this relationship is our role. When a plan sponsor hires us, they hire us to negotiate the best price for them.”
More information on other committees The Mississippi Senate and House Election Committee will discuss voter registration and voting laws on August 28
Michael Power, a representative of the Pharmaceutical Care Management Association, said pharmacy benefit managers want to make negotiations with pharmacies more transparent. Power also said there are several factors that explain why different pharmacies receive different prices.
Several lawmakers said the explanations were not good enough.
“I’ve seen things at independent pharmacists, at my own pharmacist, who couldn’t fill my prescription because it cost him more than he paid,” said Rep. Stacey Hobgood-Wilkes (R-Picayune).
What is a PBM? What other problems are there?
Pharmacy benefit managers (PBMs) act as a sort of middleman between insurance agencies, employers that pay for employees’ health plans, and pharmacies that collect referral fees. They also regulate which drug manufacturers’ products are on a list of approved products in a plan sponsor’s employee health network.
The three largest PBMs in the U.S. are CVS/Caremark, ExpressScripts, and OptumRx. They typically make money by receiving rebates and discounts from drug manufacturers for approving products and by paying pharmacies less than they charge employers and insurers. PBMs can also recoup reimbursements from pharmacies if they violate contract terms.
Earlier this year, the Federal Trade Commission released a report detailing how PBMs have incentives to collaborate more closely with their affiliated pharmacies than others, leaving local companies with no opportunity to negotiate drug prices or the terms and rates of reimbursement.
Bob Lomenick, owner of a pharmacy in Holly Springs, said one of the biggest problems for him is not being at the negotiating table with the companies.
“They give us contracts where we accept everything or we don’t,” Lomenick said. “If they get 90% of the prescriptions and send me a contract that I don’t accept, then I have a lot of patients who can’t come to my pharmacy. I’ve been working in my pharmacy for over 40 years. I’ve never, not once, been able to negotiate a contract (with PBMs).”
What solutions are currently being considered?
A bill in the 2024 session that would have addressed PBMs was rejected after interest groups representing companies in the banking sector lobbied against it, fearing the legislation would increase the cost of doing business, Waldo said.
In addition to pharmacists’ calls for greater transparency, representatives of the Mississippi Board of Pharmacies also called for stricter state laws regulating PBMs, including ways for the board to impose more appropriate fines for violations and prosecute violators.
Read about Bennie Thompson at the DNC Bennie Thompson calls on voters at the DNC to “choose democracy over Donald Trump”
“It’s just a matter of plugging a few holes here and there so it can withstand legal challenges,” said Todd Dear, deputy director of the Mississippi Board of Pharmacy.
Waldo said the committee plans to make final recommendations on how lawmakers should proceed after completing several more hearings later this year.
Grant McLaughlin covers state government for the Clarion Ledger. Reach him at [email protected] or 972-571-2335.
